 We administer rapid antigen tests for Covid-19 both to diagnose disease in members who are symptomatic as well as to screen members who are without symptoms but fearful of an exposure and want more assurance that they are not developing or carrying the disease.
We administer rapid antigen tests for Covid-19 both to diagnose disease in members who are symptomatic as well as to screen members who are without symptoms but fearful of an exposure and want more assurance that they are not developing or carrying the disease.
Tests for symptomatic patients v. screening
When a person is symptomatic (such as fever or cough), insurers will pay for the Covid-19 test for diagnostic purposes. We bill the insurer as we would for office visits.
However, Covid-19 tests when used for screening are not covered by insurance and are not paid for by the state nor the federal government. They never have been.
What we charge for Covid-19 antigen tests
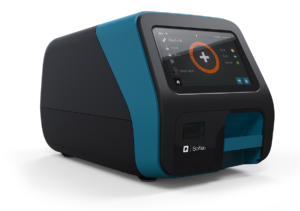
Our costs for the SARS-CoV-2 antigen test include the Quidel test kit itself and the substantial admin effort, nursing time and PPE (personal protective equipment) required.
When our members and families ask to come in just for screening, we charge $100 per test. We believe this is a fair fee and substantially lower than that charged in walk-in clinics or other testing centers. This service has been helpful to scores of members and their families.
When we screen our patients at the start of an in-office clinical visit unrelated to Covid-19, we reduce the antigen test fee to $50 because, in this case, the nursing staff involved can productively do the clinical intake for that person along with performing the test.
As explained in another recent post, we believe the antigen test, while not foolproof, provides a worthwhile additional level of safety in detecting persons with asymptomatic or presymptomatic Covid-19. This in turn makes our office a safer resource for all our members.

