As we reach Day 4 of Week 7 of the Covid-19 epidemic, we have all been consumed with the still elevated case rates and death rates in Massachusetts, as well as with our personal safety and our livelihoods. All serious concerns.
Where we are right now in our state
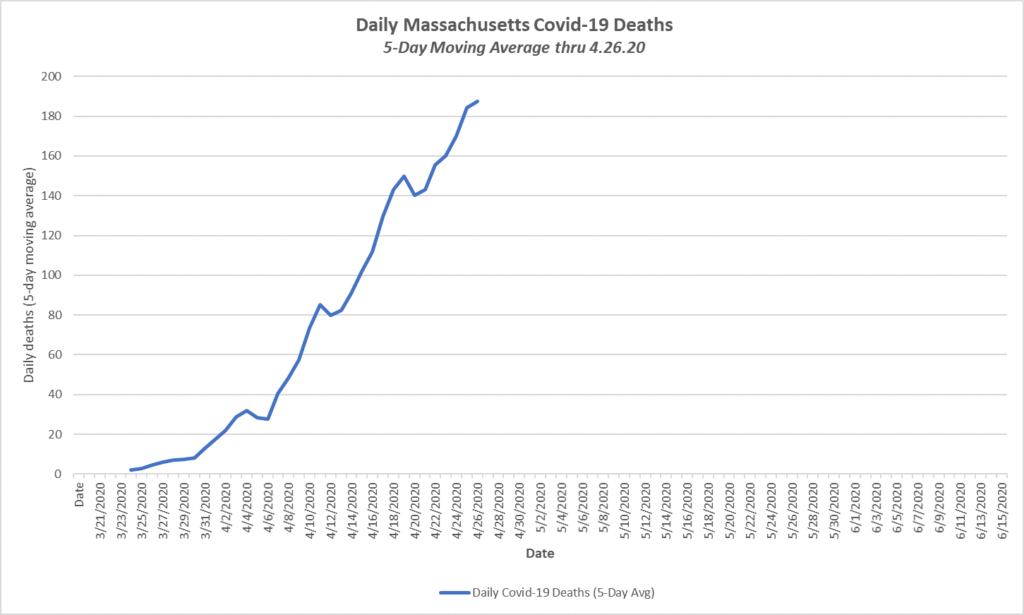
The reported deaths in Massachusetts from the Covid-19 virus have been steadily increasing and are now over 180 daily. By contrast, the average daily death rate from infectious diseases in our state in 2017 was four (4) and the average total daily deaths was 161:
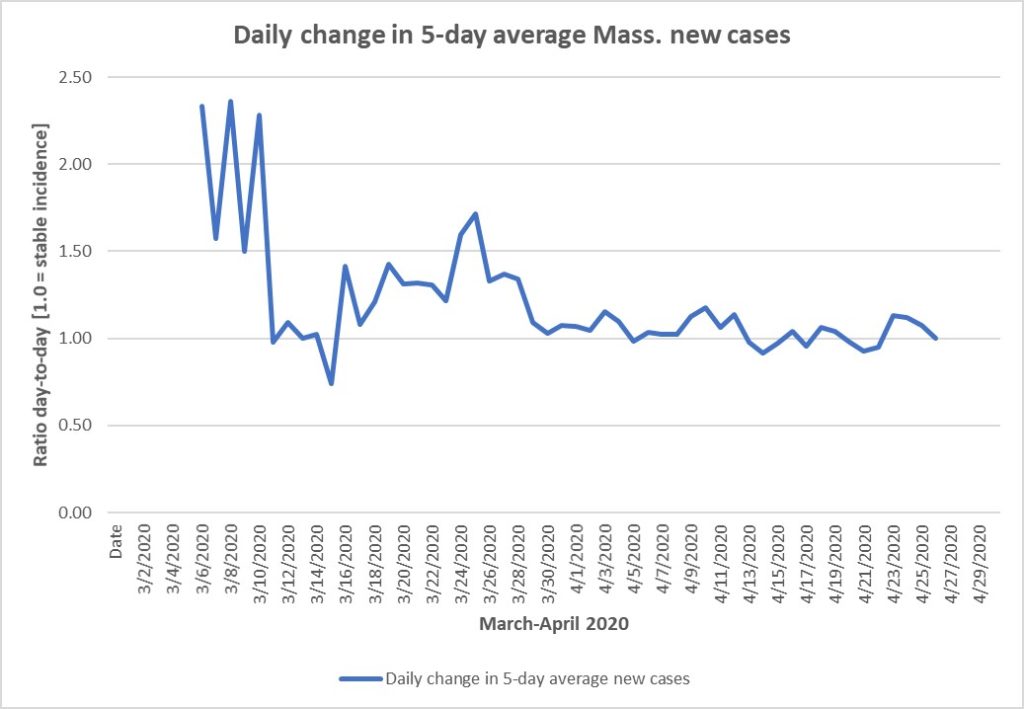
New cases remain at a high level but are no longer increasing daily, but neither are they particularly decreasing through yesterday, not to mention the retroactive addition of several thousand confirmed cases by the state to prior data because of late reporting by Quest.
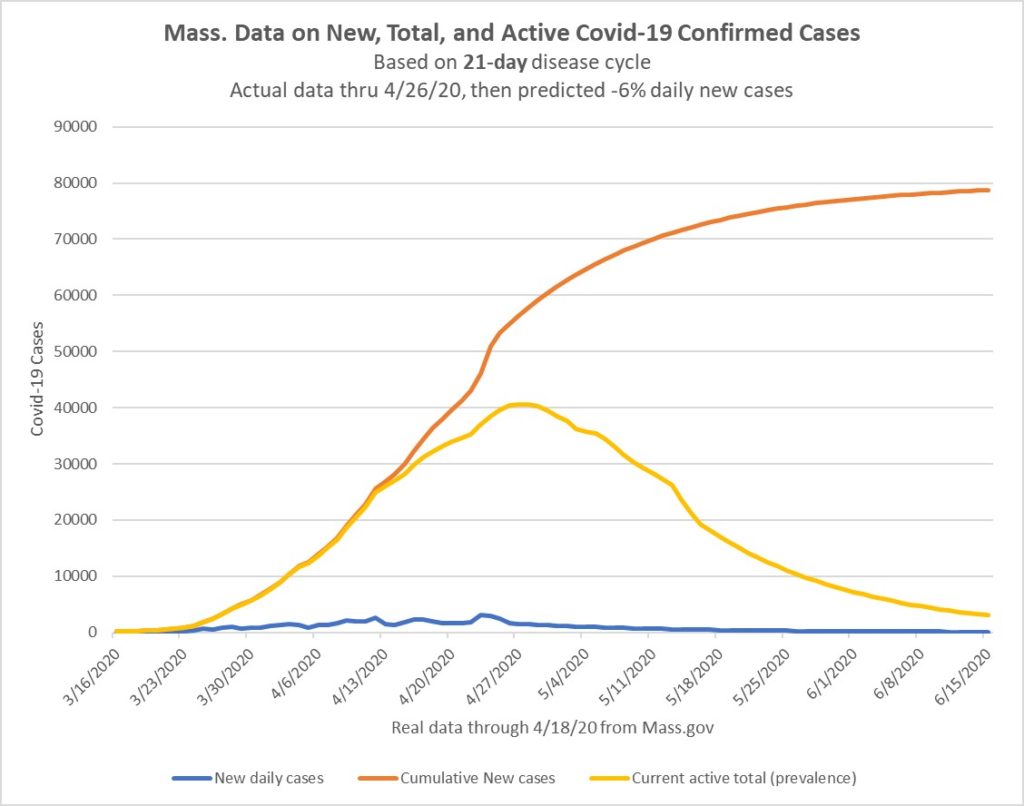
So we are more or less at a plateau because new cases levels are flat, but the total number of cases (prevalence) will continue to grow because we continue to generate far more new cases than the number of cases from 21 days ago that have completed their course and no longer have active disease. For example, the five-day average of new cases yesterday was 2334. The number of cases dropping out on 4/1 was 1176, almost exactly half the new ones.
We will need to see (and indications have been that we will see) a reduction in the daily number of new cases in order to be able to see a decline in total active cases. Allowing for a 6% daily decrease in current cases (that I have been using for reasonable if a bit simplistic estimation of the rate of decline), we may begin a slow decline in prevalence by the end of April, although we will certainly need till end of May or early June to get down to low levels in the state. I believe this is consistent with most of the more complex models and predictions:
How can we and should we think of risk?
The Covid-19 disease and its distribution and risk to different locales and individuals is immensely complicated to analyze and explain. I will do my best to highlight the underlying themes we need to consider, with emphasis on the inherent uncertainties in all medical tests. I promised myself (for you) that I would also be brief, but I am not sure that I will achieve that goal. We should first review quickly how we diagnose a disease and the role of testing.
How do physicians make a diagnosis?
Physicians make medical diagnoses based on the history or story of the problem as told by the patient or observed from the environment, by physical examination (some of which can be done by video), and by testing, both lab tests and imaging of many sorts. A single lab test is usually only part of the diagnosis, though often an important part. We analyze and organize this data to arrive at a medical conclusion, or diagnosis, as to what the condition is, usually with some understanding as to the known cause, and hopefully with knowledge of some treatment, preferably one that reliably works.
In the case of Covid-19 this process may be difficult and uncertain. We all have heard the “usual” story of onset of cough, shortness of breath, fever and malaise, but hardly everyone gets those symptoms. Fever sometimes doesn’t come till well into the illness. Some people initially have primarily sore throats without cough. Others sometimes mainly intestinal problems including diarrhea. And many other variations. And most important, the CDC (Centers for Disease Control and Prevention) has documented that sizeable numbers of people with documented Covid-19, especially including children, demonstrate no symptoms at all. So the strength of the history in making a Covid-19 diagnosis is really reduced, even when we focus on details of possible exposures.
What are the tests for active Covid-19?
You all have heard of the annoying nasal swab to get a RT PCR test for active infection. RT stands for reverse transcriptase. PCR stands for polymerase chain reaction, a method of amplifying the viral RNA picked up on the nasal swab, to allow confirmation that the virus is present. This is currently the “gold standard” of detection for active cases of Covid-19. You all also know how hard it has been to get such testing for the past two months, with most testing restricted to actively ill patients with suggestive respiratory syndromes. We are still weeks or much more away from getting such a test on anyone who is modestly ill or with no obvious exposure.
The restriction in testing is not because it would be wrong or unhelpful to test more widely, or just because someone was worried (sometimes tests are therapeutic not just diagnostic, by the way), but because we remain shamefully lacking in testing capacity. No other biological test in my memory has ever been unavailable or restricted as the Covid-19 PCR.
How useful is the PCR test?
However, we need ask how good is the PCR test for diagnosing or excluding active disease? The short answer is that, if the test is positive, it likely confirms that you have Covid-19, certainly if you have compatible symptoms. There are not many false positives. If we had the ability to test all the population, this would clearly be the way to ferret out all the infected people who are without symptoms (they exist in real numbers) so they could quarantine themselves. That would be immensely useful, but can’t happen since we lack the testing capacity. Any other method of testing (there are others underway) that reliably located antigens of the active virus (rather than RNA) might serve this screening role for active disease, if such tests were widely available. Keep tuned.
If, however, you test negative by PCR, then the answer is much fuzzier. Reports from China and elsewhere worry that up to 30% of people who have the Covid-19 syndrome and appear ill may falsely test negative by PCR. The diagnosis of Covid-19 may still be made, however, based on history and physical findings and chest CT and so forth, since the lab test is only part of the information.
What about those PCR false negatives?
The false negative rate really comes into play if you desire to clear people as free of active disease so they can return to work, or for you to socialize with them in small groups, or visit grandma, and so forth. Being certified free of active disease is immensely useful. It is also difficult to achieve. Why?
If the PCR specificity (ability to accurately identify currently infected and contagious people) is well less than 100%, what do you do? You can test repeatedly in a short period. If the specificity is 70%, then 30% of the time an infected person could test negative. If you repeat the same test, the likelihood of two successive false negative tests is 0.3 x 0.3 or 9% (o.09). Is that acceptable, a 9% chance of infection in someone said to be clear? Probably not. It takes two more or a total of 4 sequential PCR tests at 70% specificity to get the risk of being wrong below 1% (0.3*0.3*0.3*0.3=0.008 or 0.8%). If you are happy with that level of risk (1% chance of being wrong), then you are okay. But even if the false negative rate is only 10%, single negative PCR tests are unlikely to assure people that they are reliably free of disease, especially not when the stakes are high (such as interacting with highly vulnerable older relatives), without considering the overall exposure context.
For the record, medical staff are being cleared to return to work at most hospitals after two (not four) PCR tests. That would suggest a specificity of 90% for the PCR tests to hit a 1% risk of false negative after two tests. It is hardly clear that the tests are that good.
This exercise was to explain why PCR tests are not our saviors, even though their lack of availability remains an embarrassing debility. Currently single negative PCR tests, devoid of context, are weak data, although positive results offer solid confirmation in the context of apparent disease.
What about antibody testing?
Antibody testing will eventually be useful but how and when is fuzzy, like the PCR data. After exposure to a viral disease, our bodies develop early antibodies of a specific class, called IgM, that appear in perhaps 10 days and last 3-6 months, and later give way to long-acting IgG antibodies, that may start as early as 6 weeks or so and can last a lifetime. Knowing the presence of IgG or IgM antibodies to Covid-19 certainly could be immensely useful. But, again, there are still issues.
First, the accuracy of the current crop of antibody tests, which we have all just begun to hear about, is questionable. The New York Times just reported 3 days ago on an independent scientific analysis of 14 different antibody lab tests, none as yet approved by the FDA but allowed on the market by an emergency exception. The disappointing result was that 11 of the 14 were grossly inaccurate and unusable. These did not include a newly announced Quest Diagnostics test, but the same concerns have to apply to that as well until further validation data by experts is available. An unreliable antibody test, whether positive or negative, is worse than nothing.
Second, even if we had accurate results of IgG testing, it is still not known whether IgG antibody is actually protective against reinfection. This is the crucial issue. The World Health Organization and our CDC continue to identify that as the critical issue to be resolved in order to deploy IgG testing for epidemiological purposes and for decision-making. The obvious import of having protective IgG antibody would be the ability to go out, circulate and work and socialize without worry. In reality, though, most people are expected to test negative since epidemiologists think that a relatively small proportion (? 5-10%) of the whole population has been affected so far.
Third, if it were accurate, IgG testing would be intellectually satisfying to confirm that a prior case had in fact been Covid-19, even if antibodies prove not to be preventive. But the tests still have be to known reliable, and they are not yet. When antibody tests are reliable, we certainly will recommend that most patients get them to learn where they stand, perhaps even before it is definite as to the protection they provide.
Opportunity to help validate an antibody test
If you want to help in the validation process of a new, quantitative IgG/IgM antibody test, specifically by providing a fingerstick blood test, your help would be welcome. An Orchard Health Care member, Andrew E. Levin, Ph.D., is the president and scientific director of Kephera Diagnostics LLC, which is working to complete the validation of their ELISA antibody test, which has preliminary approvals. While they are primarily looking for people with PCR confirmed Covid-19 (who are exceedingly few in our practice), they may soon be interested as well in testing people who clinically appeared to have Covid-19 but could not get PCR tests. There are a number of members like that. A flyer attached explains what they are doing and how to contact them.
Managing your risk in face of uncertainty
Enough of all the uncertainties of exposure, testing and so forth. Life is uncertain. This disease is uncertain but clearly worrisome. Next week will be different. What do we do now?
Let’s summarize the environmental risks, the biological risks, what personal defenses we can invoke, and then what our personal safety strategies might be.
First, I want to list important components of the environmental risk framework:
- Densely populated areas near Boston and elsewhere are generally more affected than western Mass. rural areas, and Massachusetts has higher overall infection rates than most states
- Dense living conditions (nursing homes, assisted living, rest homes) and downtowns are much more affected than suburban and rural areas. Nursing homes and related eldercare facilities account for around half of all cases and deaths
- Infection rates appear highest in prolonged close social contact with others especially indoors (think conference rooms, auditoriums, also restaurants, churches and family gatherings). Distance matters, hence the 6 ft standard.
- Brief passing contact and outdoor contacts have little risk of spreading the virus (duration of contact matters)
- CDC recently confirmed that infected people can be contagious for at least 48 hours before they are symptomatic, and people can also be contagious and never be symptomatic. While the numbers may be small, it is clear that the lack of a cough or fever does not mean another person is free of disease. The hidden illness makes assessing the risk much more difficult.
- Inanimate objects such as mail, cartons, or your groceries all have low risk of passing the virus, although hard surfaces in public places are suspect
- Currently there is no effective therapy for Covid-19, though countless companies are working to find one (it is not hydroxychloroquine or bleach)
- Currently there is no vaccine for Covid-19, though an Oxford University group apparently is close to a human trial (light speed in terms of vaccine development)
Second, the biological risk is not uniform. CDC as well as world data are clear on this. As of yesterday 958,000 Americans were confirmed with the disease:
- Children are rarely seriously affected
- All age groups are affected, most recently of the total cases so far, 2% were under 18, 35% were 18-44, 35% were 44-65, 11% were 65-74, and 12% 75 or older (CDC data)
- Severity increases with age, with greater hospitalizations, ICU need, and deaths with increasing age especially after age 65-70.
- Significant underlying diseases make for greater severity and death at any age. These include active heart and kidney disease, insulin-dependent or poorly controlled diabetes, chronic obstructive lung disease and obesity, but do not clearly include well controlled high blood pressure or preventive drug programs to prevent heart disease.
- Immunosuppression with Enbrel or comparable biologicals for rheumatoid arthritis, psoriasis, Crohn’s disease or multiple sclerosis likely are a risk for more severe Covid-19 disease, but that is not necessarily an indication to forgo such treatment.
- In addition, anyone at any age can potentially have a severe and overwhelming case of Covid-19, where the exact susceptibility is as yet not known.
- CDC recently confirmed that people who are infected can be contagious for at least 48 hours before they are symptomatic, and people can also be contagious and never be symptomatic. While the numbers may be small, it is clear that the lack of a cough or fever does not mean another person is free of disease.
Third, what personal safety measures can we take in the absence of a vaccine or preventive medication? These issues have been much discussed:
- Staying at home in quarantine, more or less, avoids external contact with any Covid-19 risk of an infected or unknowingly infected person. But we don’t want to do this forever. It is getting pretty long already.
- Frequent and careful handwashing works well against the virus. Purell is an acceptable substitute if soap and water not available or convenient.
- Careful social distancing of at least 6 ft indoors or out, preferably a bit more indoors, should be effective. It is not completely clear that simple distancing is truly protective for prolonged lingering in an indoor space, even with a standard surgical mask.
- Wearing masks when encountering others is likely to be mandatory for some time, but which mask matters, and our mask supply is limited.
- Surgical or procedure masks protect others from you but are not really secure against incoming air streams in close contact. These are still in short supply though some people have been able to get them. They are probably the best available for the moment.
- N95 “respirator” masks provide the most secure protection against infection, and are now worn by all medical personnel working with Covid patients, but they have been and remain exceedingly hard to obtain. We are still trying to get an adequate supply for our office after two months. I think this should be the target mask for everyone once they finally become available.
- Cloth face masks may offer some protection for others, and perhaps some for you for low-threat encounters (a quick run into the pharmacy to pick up something), but they are a thin reed on which to base your safety in any close contact situation. As soon as supplies of surgical masks or N95 improve, the hand-made masks should be retired.
- Eye shields are worn by medical staff in any close encounter with a patient with Covid-19. These are little talked about, but the virus can infect (according to CDC and other data) by landing on the cornea and eventually finding its way to the nasal passage through the tear drainage system. Close contacts with infected people do carry risk of infection through the eyes.
Importance of better PPE to mitigate enhanced risk
I want to emphasize the potential importance of seriously effective face and eye protection as part of an eventual repertoire for our own self-protection as we consider our emergence from hibernation later this spring. The CDC emphasizes both face and eye protection for front-line health care workers, but unlike N95 respirator masks, eye protection has received little public comment.
In a CDC guidance this month directed toward health care personnel working with Covid-19 patients, the document (Interim U.S. Guidance for Risk Assessment and Public Health Management of Healthcare Personnel with Potential Exposure in a Healthcare Setting to Patients with Coronavirus Disease 2019 (COVID-19)) made clear that N-95 masks were clearly better protection in close quarters with an infected person than was a plain surgical mask, and also that eye protections (shields or goggles) had independent benefit of protection.
In fact, their table of exposure risks fact elevates the seriousness of any close exposure to an infected patient (direct contact, aerosol-producing procedures) by one level, from low to medium risk (requiring 14 days quarantine) for wearing a surgical mask and not an N95 respirator, and establishes a medium level risk in close physical patient contacts (think massage parlor workers) who don’t have an eye shield.
While these risk evaluations and PPE advice related to health professionals dealing directly with Covid-19 patients, the issue relates to everyone. The CDC recommends elevating the level of personal protection equipment in response to a higher risk of exposure, in order to reduce the combined risk of a Covid-19 infection and adverse personal outcome for the average healthy health care professional.
Similar analysis promptly suggests that one could and should elevate one’s level of personal protection at any given level of exposure if one is either at higher risk of infection or of suffering a worse outcome if infected. The CDC advisory specifically points to better masks and eye protection as key tools of greater self-protection.
My suggestions to thinking about your own risk profile
Everyone must remember that, ultimately, anyone you meet for many months could be an asymptomatic carrier or presymptomatic victim of Covid-19. The only questions is how widespread this asymptomatic disease is, which we hope to learn by community test sampling over the next few months. This is why “universal precautions” for everyone’s protection are what is needed, implemented through social distancing and masks.
- Everyone should plan to practice careful social distancing for the foreseeable future. Six feet is minimum. Outdoors is less risky. Masks must be worn in any close encounter, however brief, as part of social distancing. Of course careful handwashing. Gloves do not appear to be essential if you wash your hands carefully after any exposure.
- Additionally, everyone should also give careful thought before lingering in any inside space with any group, even if separated and wearing standard surgical masks. While separation and a plain surgical mask appear to work well for healthy people in short encounters (like going through super markets), I am personally skeptical that the same is true of long stationary stays in a room. I can’t imagine, therefore, how dining in restaurants can safely return in coming months. Fortunately the summer months will enable safer outdoor social contact.
For younger and middle-aged healthy people, the effective safety from social distancing and plain surgical masks (and in some brief circumstances, a cloth mask) may be sufficient protection to lower your risk level compatible with your lower risk of developing serious disease from Covid-19. Similarly, eye protection may not be needed for you in general, because of the lower risk of severe outcome from a Covid-19 infection.
For older members (over 65 even if vigorous, as most of you are) and for anyone on any immunosuppression, you should carefully think about your risk profile. Data show that you are more likely to have a severe course with a Covid-19 infection should it occur, and those who are immunosuppressed are also more likely to contract the infection. So your defensive posture should be higher to mitigate your enhanced risks. The goal is to keep everyone out of hospital or the ICU.
To me this means that older or immunosuppressed members should use stronger PPE when out, specifically trying to obtain N95 masks (like medical workers) as your protection norm. And you should strongly consider some sort of face shield, which could be worker’s goggles from Home Depot, for any prolonged encounters even with social distancing and the N95. I would also be reluctant to engage in closed room social gatherings with any lingering, even with that protection. I am essentially suggesting you adopt these higher protective barriers (like general medical staff) to protect you against the unknown but still present Covid-19 exposures since you are more susceptible and since the outcome of infection is likely to be more serious.
In conclusion
I have tried to walk you through multiple, some rather complex issues with the Covid-19 epidemic, starting with where we are in the infection epidemiology and then exploring the types and efficacy of biological tests, and winding up with discussion of differential personal risk and differential possible responses in behavior and personal protective ingredients. My apology for the length of this discussion. I tried to keep it short, but ultimately chose clarity over brevity. I hope you see it that way as well.
Comment and questions are welcome.


Question – is wearing sunglasses outside any protection at all?
Sunglasses will provide some direct splash protection, but outside the real protection from Covid-19 exposure is distance and gentle airflow. I wouldn’t see any frequent indication for goggles or a formal eyeshield in outdoor activities. And sunglasses protect your eyes from UV light. Again, outside is healthy for us all and low-risk for any kind of adverse viral exposure.
Dr. Kanner,
Thanks for all the detailed analysis you’ve been posting.
Can you comment on the study cited in this article?
https://www.npr.org/sections/goatsandsoda/2020/04/22/840146830/adding-a-nylon-stocking-layer-could-boost-protection-from-cloth-masks-study-find
Seems as if this might be a way to get closer to N-95 protection before that is readily available to the public.
Thanks.
Cliff
Cliff, this is a great article that explores how a layer of nylon stocking around the face under a cloth mask improves the effectiveness of the mask, as well as improving N95 masks. There is both better filtration and closer adherence to the face for better air seal.
I am all in favor of improving masks and have no pretensions to being a mask designer or evaluator personally. I am clearly in support of the wide use of effective face masks that are comfortable, compatible with exercise, and available.
I think the N95 effectiveness level is the target for everyone’s protection, since standard surgical masks have tested much more poorly (look at the CDC exposure guidelines). I am totally in support of improved cloth masks (by any means) that offer better protection than the typical surgical or cloth mask and more comfort than the typical N95. Bravo to anyone and everyone who designs or produces such masks.
The nylon stocking section is to be worn OVER, not under the mask – its purpose is to hold the mask more tightly to the face, to minimize gaps around the sides and tops. The nylon itself has little filtration capability.
Thank you for this. Very well written! You are amazing.
Allen and I are hoping to drive home from Florida at the end of May or early June. It’s a long drive. Would you feel safe using public rest rooms? Staying overnight in a hotel? Even if we fly jet blue stopped all direct flights from palm beach to Boston. We would have to fly from ft lauderdale and that means taking Uber’s and flying from a busier airport and more crowded planes. What is your advise on this?
I would drive, take sanitizers, stay in a hotel. You can control your environment that way and do extra wipedowns in the hotel if need be. That’s much more controllable and quite low exposure compared to flying and going through airports. It’s not that the airlines aren’t trying to clean up the cabins. It’s the potential uncontrolled actions of fellow passengers or those in the terminal that could put you unexpectedly at risk. The drive is manageable and might be interesting. Have you ever done it?
Never done the drive. Planning for 2nd week of June as of now.
Do eye glasses provide any kind of protection?
Betty Gitlin-Rich asked the same thing earlier. Some protection, but not real protection if you are in any close quarters. But the eye risk is low except in close quarters.
If most transmission occurs indoors (especially at home especially among inactive elderly folks), wouldn’t I be wise to go outside a lot. Walk the dog? Prune fruit trees?
Are you wildly understating the effectiveness of fabric face covers? Full Disclosure: I make 10 million a day—roughly 10% of US demand for non-N95 masks. There is not enough capacity to satisfy demand for fabric face covers. Get used to seeing them. You’ll be seeing a lot of them in the coming months and maybe years. The N95 mask’s power of limiting penetration of 99.98% of 0.1 micron rubber spheres comes at the price of breathability. If you are planning to walk briskly, an N95 will feel like breathing through a straw, unless it doesn’t fit. If you look for TV commercials showing medical personnel just having removed some N95 masks, you’ll see indentations at their cheekbones where properly a applied mask compresses flesh to achieve a seal. Most of the rest of us don’t achieve that seal with N95 masks or conventional fabric face covers and air mostly moves up and down a gap between the nose and the cheek. That passage of air almost totally defeats the N95 mask as well as cheap, durable, rigid plastic masks. The virus doesn’t float freely. It is inside droplets of water which do not penetrate most fabric and definitely not the specially coated papers in N95 masks. If your mask fogs your glasses, it’s not working. Also throw your mask away and then immediately wash your hands. Your breath contains a lot of virus—flu, cold, etc. (although fresh air contains comparatively none). Your mask should be “grab and go, and then get rid of.” For most of us to be disposable something needs to be cheap. Reusing an N95 mask in not recommended. Please note, I didn’t pitch my mask, but it’s really good—soft, fits well, comfortable and (surprisingly) effective.
Want some advice beyond going outside (rather than the conventional advice of “staying home,” washing your hands, etc.) Avoid people who aren’t wearing fabric face covers outdoors and indoors (especially). Workout to build a little muscle—it might come in handy. Eat better. Eat less especially bread, rice, pasta, potatoes, and sweets. (Only political correctness keeps us from calling obesity a pre-existing condition). Learn to cook (and bake). Share your creations with your neighbors or the refreshments table after church.
For a pandemic, this one, in truth, is only a bit more brutal than the seasonal flu. Yes, it started off at a terrific pace—cases and deaths increased 10-fold each week for weeks. At that rate, in a little over three weeks everyone—7 billion humans—should have had it. We don’t—-not due to a vaccine or a preventative treatment. We don’t because we have immune systems. Apparently 15% of us have antibodies suggesting we’ve had this new-to-humans disease since it flew here on a jet plane in January. On the news, you’ve seen one million Americans have the “confirmed cases” of this disease. That’s 0.3%—-1/50th of what various antibody tests find. We anticipate 60-70 thousand Americans will die of it—0.02% roughly twice the mortality rate of seasonal flu last year or the year before. Your risk is more like 0.01% if you aren’t in a nursing home and lower still if you have none of the pre-existing diseases (of which obesity seems most common). Oh, yes, what about the rest of us? You know, the 85% who appear vulnerable because we haven’t become confirmed cases nor do we have the specific antibodies? We’re likely fine—not so fine I don’t wash my hands a lot and wear my fabric face cover where I might run into others. Our immune systems are pretty aggressive. COVID-19 is a new coronavirus for almost all us who don’t consort with bats or Asian zoo animals. The common cold can be a coronavirus although it’s mostly a rhinovirus. Perhaps, admitted I’m speculating here, our immune system has bits and pieces that aren’t perfect for dealing with COVID-19, but good enough.
Once this pandemic is over, thank your immune system and devote more time to strengthening it. Go to the beach. Get a tan. Eat your vegetables. Get in close contact with other healthy people and animals again. Make new (younger) friends. Buy less. Work as much as practical from home—read and take calls outdoors.
If a vaccine appears ask Dr Kanner whether the risks outweigh the benefits. Remind him of the 1976 swine flu vaccine that got pulled back after people started developing Guillain-Barrė Syndrome.
Tom, I am awestruck by your rapid startup to produce the volume of masks you are. I would be immensely pleased if cloth masks could provide the requisite level of protection for large portions of the population. We certainly aren’t getting adequate numbers of N95 masks soon.
My concern has been, first, that various tests I had seen a few weeks ago of the effectiveness of cloth masks and of surgical masks, compared to N95, were troubling and appeared to show substantially less protection. I unfortunately did not archive the articles that I read on this. As people validate mask effectiveness, or look to enhance it (as was suggested by the NPR article cited by Cliff Romash earlier), I will certainly be a supporter.
My second issue is that I believe (and explained) that the populations at higher risk of becoming infected or succumbing to infection, namely the older or immunosuppressed population or people with substantial comorbidities, logically should use a more effective mask to achieve a lower risk of infection compared to the general, healthy population. That can be achieved by better masks and perhaps the addition of eye protection in those settings that are more risky. That extra protection is not really needed outdoors; I totally approve and encourage everyone to get out, walk and run, enjoy the sunlight, eat healthy.
We will all learn more when we finally get community sampling data to validate whether 3% or 15% of the population has been exposed. That critical point is disputed, and certainly may vary in different parts of the country or a state. The data so far may also reflect inadequately specific antibody tests that were actually picking up all coronavirus exposure not just SARS-CoV-2 antibody. I hope you and others are right, that there is a wide exposure already in the community, since that will mean, as you said, that the morbidity and mortality of Covid-19 are really much milder than has been perceived, and that we are much farther along to realistic community (herd) immunity that we thought. I don’t think we have that answer nailed down at this point.
Thank you so much for sharing what you are effectively doing to provide cloth masks and your thoughts on the effect of this disease on our society.
Ongoing research into the use and possible reuse of N95s is showing that the virus can live in the material for up to seven days, as compared to two days for cloth masks. Kirsten Koehler, an associate professor of environmental health and engineering at the Johns Hopkins Bloomberg School of Public Health, suggested that healthcare workers could each keep seven masks, and use them in rotation. Each mask would be placed in a paper bag each day, the bags labeled by day of the week.
Unfortunately, the antipation that “60-70 thousand Americans will die of it” is turning out to be an underestimation, and that underestimation is growing by nearly 2,000 people each day. From the CDC page
“TOTAL DEATHS
96,002
1,852 New Deaths*
*Compared to yesterday’s data”
Doubtless we would most likely have many more people die of the flu, if we didn’t have vaccines, though. However, the disease is much more deadly to the elderly, because the immune system actually declines in effectiveness as we age (although people who are very active will have better immune function than their inactive peers, certainly!) and the elderly are much more likely to suffer the “cytokine storm” effect, which can cause a wide variety of secondary effects, ranging from neurological damage to organ shutdown. This is not an effect that’s strongly associated with influenza.
Thank you, Dr. Kanner and Dr. Sobel, for keeping everyone informed re Covid 19 risks and mitigation procedures. Your understanding and relating it in terms that non medical individuals can try to understand is greatly appreciated. Sounds as though everyone should make an effort to obtain N95 masks to really be safe when going to grocery stores and pharmacies. Thank you. Margi and Dave Doherty
Margi and Dave, I think grandparents should have a higher level of mask protection in all environments, given their enhanced risks, but N95 masks are hard to come by and a quick shopping experience at a Star Market or Whole Foods is relatively low risk. So practically, a standard surgical mask or a cloth mask may be sufficient. Tom Meyer below is making cloth masks and offers useful thoughts. I hope we will get more independent evaluations of cloth masks and enhancements so we can rapidly achieve a sufficient supply of more effective masks of any sort to ease this shortage situation.
Thanks Dr. Kanner. This note is meant to be additional information for all readers. Cloth masks aren’t the best solution, but when almost everyone wears one, it is an aid. That said, it is astonishing to see people who wear fabric masks but do so in a way that prevents the mask from being helpful at all. I have noticed people of all ages doing very silly things with masks.
What is not helpful is when people wear the mask improperly or wear a mask that is too bid. Make sure that when you wear the mask, that it is tied in two places or the elastic loop goes completely around the ear. Make sure the mask covers the mouth and nose. (No kidding, twice in 10 minutes I saw individuals with the mask pulled down below the nose.) If the mask is too big, there are three possible ways to get a better fit. 1. Make a knot in the elastic bands, 2. Take a piece of webbing or double thickness of fabric and sew a button on each end. This “device” goes at the base of the skull and between both ears. Wrap some of the string/elastic from the mask around each button. 3. For elastic bands that go around the ear and the mask is too big, string a shoelace through each elastic band, pull the bands closer together with the shoe lace and tie a knot with a bow to hold the elastic bands closer together.
Marcy,
Thanks for the detailed and practical suggestions to wear a mask properly. I also am amazed to see people use masks of any sort below their nose. Especially when they are shown on TV!
I live in housing for the elderly, and I’m amazed at some of the idiots that live in my building! One woman was, as mentioned above, wearing her mask beneath her nose. I said to her “You know, the mask is not going to help you if you wear it like that”. She said “I can’t wear it up over my nose – I can’t breathe!” The next time I saw her, she had the bottom strings tied snugly around her neck, but the upper strings were tied loosely, so that you could clearly see her nose and mouth from the sides! I didn’t say anything more to her about it – I just give her an extra wide berth if I see her!
Great message…very thorough and interesting. What do you think of today’s report in the NYTimes of the Oxford vaccine prospects? And what do you think all of this is going to do to the structure of US medicine, and old folks homes?!
Anne,
I am quite interested in the Oxford vaccine effort as reported briefly in the Times, although I don’t know details. If they have a novel method of finding a component target and design the vaccine, this would be the fastest development effort in human history. Keep your fingers crossed.
Thanks for this and all of your blog posts, Dr. Kanner. They are all extremely clear, practical, and helpful. So much so that they have become “must reads” for everyone in our family – not just our Mom, who is the grateful client of your practice. I think you have helped many folks stay safe and healthy during the COVID-19 pandemic, and it is deeply appreciated.
Sincerely,
Steve Moore
On Behalf of the Moore Family
I am honored to be considered “must read” by your family. I try hard, in each post, to abstract and explain the essential medical themes of the pandemic at that time, including critical details, from the overwhelming daily information flow that itself is constantly evolving and often conflicting, to provide each reader with accurate, understandable, and actionable information.
You and your family and friends are welcome to sign up for these emails with the Sign Up? link on the blog pages. And of course you can simply check the website once or twice a week.